Ambulatory Services
Ambulatory Care Locations
- Pulmonary Function – D Wing, Main Level
- Infusion – D Wing, Main Level – Ambulatory Care Unit
- Women's Health Clinic - D Wing, Main Level – Ambulatory Care Unit
- EMG – D Wing, Main Level
- Fracture/Orthopaedic Clinic – D Wing, Main Level
- Internal Medicine Rapid Access Clinic (IMRAC) - D Wing, Main Level
We recommend those with an ambulatory care appointment to please park in the garage off Elizabeth Street and enter through the D-Wing entrance.
You should then register at the central registration desk in the D-Wing lobby.
Forms
- BCHS Consent to Medical Treatment Form
- Infusion Clinic - IVIG - Neurology Referral Requisition
- Infusion Clinic - IVIG - Non-Neurology Referral Requisition
- Infusion Clinic - Blood Product Referral Requisition
- Infusion Clinic - Home and Community Care Support Services Iron Infusion Order Form
- BCHS Iron Sucrose Preprinted Orders
- FIT/FOBT Positive Centralized Colonoscopy Referral Form
- IMRAC Referral Form
- Pulmonary Function Requisition
- Fracture Clinic Referral Form
- LDAP Referral Form
Ambulatory Care Services
The following information pertains to all patients undergoing procedures at Brant Community Healthcare System:
- Please arrange for a responsible adult to accompany you to and from your scheduled procedure. This person must be available to pick you up after your procedure.
-
You are advised not to drive for at least 24 hours after your procedure, preferably not until the next morning.
- Patients are advised to have someone stay with them for at least 12 hours post procedure. Be prepared to stay home for the remainder of the day.
- Do not eat any solid foods, or drink milk, orange juice, or any non-clear liquids starting at breakfast time the day before your scheduled procedure.
- Do not chew gum or eat candy prior to your procedure.
- Please remove all jewelry, make-up, and nail polish before arriving at BCHS Endoscopy for your appointment.
- Patients are advised to leave all valuables at home as we will not assume responsibility for lost or stolen property during your time at BCHS Endoscopy.
- Please complete the attached patient questionnaire form and bring it with you to your scheduled appointment. Download here.
- Bring your health card with you to your appointment.
- If you take prescribed medication on a daily basis, please continue to do so unless otherwise directed. Mention to your doctor if you take any blood thinners. Bring your medication list with you to your appointment.
|
Internal Medicine Rapid Access Clinic (IMRAC) |
|
The Internal Medicine Rapid Access Clinic (IMRAC) provides improved access to internal medicine expertise for patients with complex and complicated medical issues. If you are referred to IMRAC, you will be seen by internal medicine physicians at IMRAC one or two times to manage you acute medical issues.
When you are referred, you will be contacted with more information regarding your appointment. It is our goal to see all IMRAC patients within 3 business days of their referral. Patient appointment handout. |
|
Gastroscopy |
|
A gastroscopy is a procedure to look inside the esophagus, stomach and the first part of the small bowel. A small tube with a video camera on the end is inserted through your mouth to look at your throat and stomach. Indications for Gastroscopy:There are many indications for a gastroscopy which include heartburn, regurgitation, difficulty swallowing, anemia, abdominal pain, unexplained weight loss, etc.
|
|
Colonoscopy |
|
A Colonoscopy is a procedure to look inside your large bowel or colon. The doctor uses an instrument called a colonoscope. This is a long flexible tube with a camera and a light at the end of it. Colonoscopies are done for many reasons such as screening purposes for patients 50 years of age and older, due to a family history of colon cancer or a positive Fecal Occult Blood Test. We also do colonoscopies for patients experiencing symptoms like rectal bleeding, constipation, diarrhea, change in bowel habits, abdominal pain, weight loss, or anemia. About the procedureYou will be instructed regarding cleaning your bowel in the days before your procedure. Follow the instructions that correspond to the prescription given to you by the doctor. Sedation is used for these procedures so you will need someone to take you home. Please arrive 1 hour prior to your scheduled appointment time in order to get IV in and paperwork done. The procedure takes about 20 to 30 minutes, but you will be in our facility for approximately 3 hours, which includes your procedure and recovery time. After a colonoscopy, a nurse observes you and reviews post op instructions. Download the instructions here. Expected time in recovery is 30 minutes. |
|
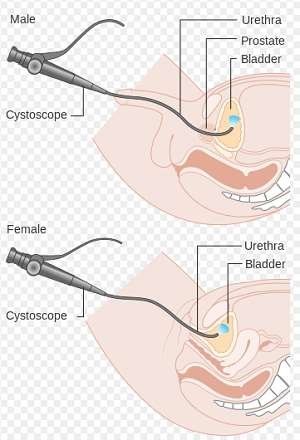
Cystoscopy |
|
Flexible cystoscopy is a diagnostic procedure to examine the inside of your bladder. It can also be used to take biopsies from your bladder, remove ureteric stents or administer Botox injections into your bladder. It is usually performed as an outpatient under local freezing. If possible, arrive 30 minutes before your procedure. You will be asked to change into a hospital gown before entering the examination room. This procedure is short and you will go home quickly after your examination. Mild burning on passing urine is common after the procedure but side effects are rare.
|
|
Minor Procedures |
|
A plastic surgeon or general surgeon performs the Minor Surgery. Patients must first be seen by a GP or family physician, and, if suitable, they will be asked to make an appointment for Minor Surgery. We have a fully equipped operating area where we aim to provide a rapid access, local service with minimum inconvenience to our patients. Before your operation
We aim to make the procedure as pain free as possible. You will be awake throughout and no sedation is required. The operation will be conducted under local anaesthetic (an injection with a very fine needle to make the area go numb). You will feel a mild discomfort for a few seconds as the freezing is administered but should feel no pain at all after that. Have a light breakfast prior to procedure. Apart from parents and carers, we are not able to accommodate companions in the minor surgery room but they are welcome to sit in the waiting room whilst you are having your operation. What to expectBefore your surgery the doctor will explain exactly what procedure is being done and why. You will have the opportunity to ask any questions about the procedure being performed and/or any alternative treatments - including what would result if you decided not to have surgery. |
|
Women's Health Clinic: Rh Negative |
|
The BCHS Women's Health Clinic offers compassionate care for women and their families. We provide a variety of specialty services for women throughout the life stages, in the fields of general obstetrics, gynecology, and uro-gynecology. Rh negative and pregnancyBeing Rh negative means that you do not have Rh proteins on your red blood cells. If your baby is Rh positive and you get a small amount of your baby’s blood into your bloodstream when you are pregnant or when you give birth, your body can make antibodies that hurt and kill red blood cells that are Rh positive. The most likely time that you would be exposed to your baby’s blood is when you give birth. Being Rh negative will not harm your baby during your first pregnancy. In subsequent pregnancies, the antibodies that you made when you were exposed to Rh-positive blood at your first birth can cross the placenta and attack the Rh-positive red blood cells, if your next baby has Rh-positive blood. This is called Rh sensitization. Rh sensitization can cause fetal anemia (low iron in the blood), miscarriage, stillbirth, or a serious illness in the baby that is called hemolytic disease of the newborn. Fortunately, Rh sensitization is very rare because women who are Rh negative can get a shot that stops their body from making antibodies to Rh-positive blood. RhoGAM RhoGAM is a medicine that stops your blood from making antibodies that attack Rh-positive blood cells. RhoGAM is a sterilized solution made from human blood that contains a very small amount of Rh-positive proteins. These proteins keep your immune system from making permanent antibodies to Rh-positive blood. They do not hurt your baby. RhoGAM is given as an injection. When do I get RhoGAM? The chance of your blood and your baby’s blood mixing is the highest at the time of birth, although that possibility is rare. However, blood mixing can also happen during the last trimester of your pregnancy, when your placenta is growing and the membranes that separate your blood from your baby’s blood are very thin. For this reason, RhoGAM is given at 28 weeks of pregnancy to protect you for the rest of your pregnancy. RhoGAM works for about 13 weeks. Soon after you give birth, your baby’s blood will be tested for Rh. If your baby has Rh-positive blood, you will get another dose of RhoGAM within 72 hours after you give birth. If your baby’s blood is Rh negative, you will not need the second RhoGAM dose. |
|
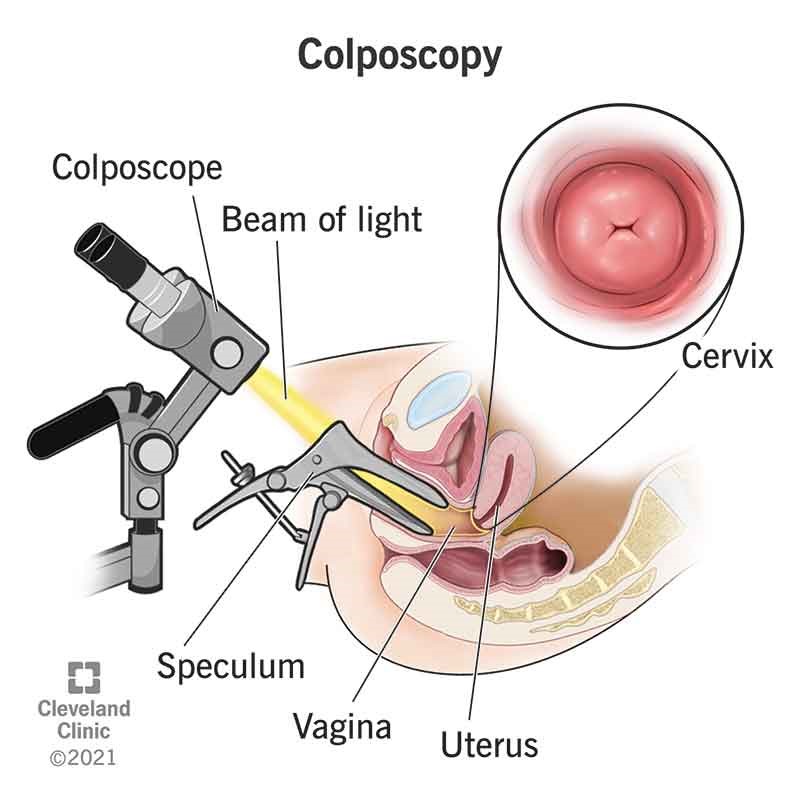
Colposcopy |
|
The Colposcopy Clinic is a specialized service for adults who have an abnormal pap test, an abnormal exam of the genitalia by a health care professional, or who need treatment for genital warts and vulvar lesions. How long will my appointment be? A typical appointment runs approximately 30-45 minutes, but this can vary. Will I have to come back more than once? In most cases, patients in colposcopy have 1 or more follow-up appointments, until the patient has a normal pap result. Does a referral mean I have cancer? In most cases, no. A common reason for referral is for dysplasia of the cervix. Dysplasia is not cancer, but does require further treatment so that it does not become cancer.
|
|
LEEP |
|
Loop electrosurgical excision procedure (LEEP) uses a wire loop heated by electric current to remove cells and tissue in a woman’s lower genital tract. It is used as part of the diagnosis and treatment for abnormal or cancerous conditions. The lower genital tract includes the cervix and vagina. The cervix is the lower, narrow part of the uterus and the vagina connects the cervix and the vulva. With LEEP, an electric current passes through the fine wire loop to cut away a thin layer of abnormal tissue. This tissue will be sent to the lab for testing. LEEP can also remove abnormal cells to allow healthy tissue to grow. LEEP may be done when cervical or vaginal problems are found during a pelvic exam, or abnormal cells are found during a Pap test. LEEP is also done to detect cancer of the cervix or vagina. Cells that appear to be abnormal, but are not yet cancerous, may be called precancerous. These abnormal cells may be the first evidence of cancer that could develop years later. Your healthcare provider may have other reasons to recommend LEEP. Generally, LEEP follows this process:
|
|
Abortion |
|
Abortion is legal in Canada. You do not need the permission of a parent or partner to have an abortion. At the Brantford Women's Health Clinic, we understand that deciding to end a pregnancy can be one of the most difficult decisions a woman will ever make. If you have made this decision, be assured that you are not alone – we are here to provide you with professional medical care in a safe, caring, and non-judgemental environment. We offer surgical and medication abortions for people who live in and near Brantford. At Women’s Health Clinic, medication abortions are available for people who are up to nine weeks pregnant. Surgical abortions are available for people who are up to 12 weeks pregnant. You do not require a referral. The clinic nurse will arrange the tests needed. Location & ArrivalThe clinic is located at Brantford General Hospital (200 Terrace Hill St.) in the Women's Health Clinic on D-wing Main. What to expect: Please present to patient registration in the D-wing 15 minutes prior to your appointment. Bring a health card. You will then be directed to the clinic for a meeting with your care team: a nurse and a doctor. Please allow between 45 minutes and 1 hour for your first appointment. The Women's Health Clinic is a small, multifunctional clinic. Abortion consults are only done one day per week. Download the pre-consultation questionnaire. Hours of operation:
Contact us:
|
|
Postmenopausal bleeding |
|
If you have gone through menopause, you shouldn’t have any bleeding. Menopause means you haven’t had a period in at least one year. If you have any bleeding, even spotting, you should see your doctor. They will rule out causes. Postmenopausal bleeding can be caused by a number of conditions. The most common causes are: Polyps: these tissue growths appear inside your uterus or cervical canal, or on the cervix. They are usually not cancer, but they can be the cause of bleeding. Endometrial hyperplasia (thickening of the uterine lining): After menopause, you may have too much estrogen and too little progesterone. As a result, the endometrium gets thicker and can bleed. Sometimes cells in the endometrium can become abnormal. Next steps:Transvaginal ultrasound: A small probe will be placed inside your vagina. It sends off sound waves to create a picture of the inside of your body. Endometrial biopsy: the doctor uses thin tube to take a small sample of the tissue that lines your uterus. They will send it to the lab where they look for anything unusual, like infection or cancerous cells. |
|
Infusion Medicine |
|
The Infusion Medicine Clinic provides adult medical treatments such as blood products (IVIG, Blood), intravenous (IV) medication (Iron, first antibiotic) and phlebotomies (treatments that remove blood). Preparation:
What to expect:
PhlebotomyThe blood is withdrawn as a treatment for certain medical conditions. This is called therapeutic phlebotomy. It removes extra red blood cells, unusually shaped red blood cells, or extra iron in the blood. The first step to getting blood drawn will be a lab test draw to see if the phlebotomy is needed. The results can take up to 30 minutes. Then, if needed, the nurse who takes the blood will ask you to make a fist with your hand. They will tie a band, called a tourniquet, around your upper arm. This makes your veins pop out a little more, which will make it easier to insert the needle in the right place. You may feel a pinch or sting when the needle goes into your arm. The needle will be attached to a small tube that lets your blood flow into a bag. Blood transfusionA blood transfusion is a routine medical procedure in which donated blood is provided to you through a narrow tube placed within a vein in your arm. The nurse will draw the lab test required to see if you need the transfusion. The results can take up to 30 minutes. The patient can arrange to come in the day prior to get the test done. An intravenous is started, consent obtained, and vital signs are taken as you sit in a reclining chair. The blood is started slowly for first 15 minutes then increased to the ordered rate. Iron transfusionIron is an essential nutrient that provides oxygen and energy for bodily processes. When your physician decides you require an Iron transfusion, a referral is sent to the BCHS team. You will receive a prescription for the iron to be filled at your pharmacy and brought to your appointment.. Iron is an important part of haemoglobin (Hb), which is the red pigment that gives blood its distinct colour. Haemoglobin is the substance that carries oxygen around your body. Iron is a key component of enzymes involved in manufacturing energy in the muscles. Lack of iron, known as iron deficiency, has many symptoms including: fatigue, tiredness, exhaustion, trouble sleeping, poor thought processing, brain fog, anxiety, depression, restless legs, hair loss, shortness of breath, heart palpitations, paleness and pica (craving ice/paper/soil/other non-foods). IVIG Intravenous Immune Globulin is a blood product that contains antibodies in a concentrated form. It is made from plasma collected from human blood donors. IVIG replaces antibodies where levels are low which helps to treat conditions like autoimmune diseases. Sometimes you will require blood work prior to infusion. Once results are in, the nurse will follow the doctor’s instructions. Consent is obtained. IVIG is a clear liquid given through an IV (intravenous) slowly over several hours. The nurse will monitor your vital signs during the infusion. |
|
Fracture Clinic |
|
Brant Community Healthcare System's Fracture Clinic provides consultation, fracture management (including casting and splinting) and surgical follow-up care. Patients are referred to the clinic after a visit to the Emergency Department visit, after surgery or as new consultations. The Fracture Clinic team also includes orthopedic surgeons and orthopedic techs. Fracture Clinic Hours are Monday to Friday 8:00 a.m. – 4:00 p.m. What to expectPlease bring your health card and register in the D-wing entrance. At this appointment wait times will vary, plan for at least one hour and up to 3 hours. FAQWhy am I waiting?
Why are some patients called before me?
Does OHIP cover all my care costs? Not all equipment and supplies are covered by OHIP. Some things that are not covered include: wrist splints, air casts, and fiber glass casts. Your extended health care coverage (private insurance) may pay for these. The Orthopedic Technologist will provide you with a detailed bill for those items that are not covered. Caring for your cast and splintYou have received a cast or splint as part of your treatment for the injury you sustained. The following is general information and specific things you need to do to help in your recovery. If you have any concerns at all, call your orthopedic/plastic surgeon, or your family doctor, or return to the nearest emergency department for assessment.
If you have a problem with the cast, call (519) 751-5544 ext 2500, and you will be assisted by an orthopedic technologist. |
|
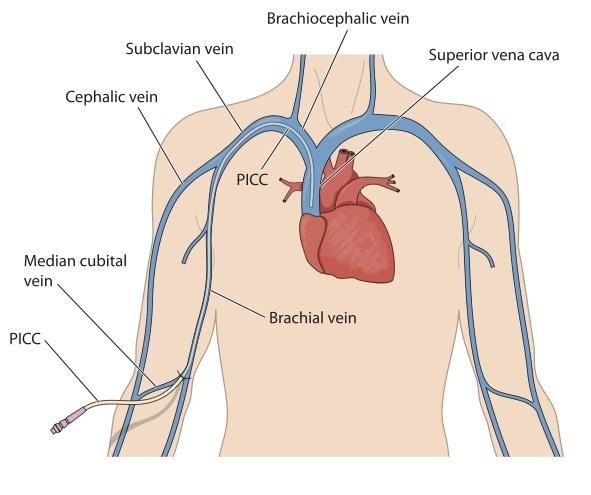
PICC |
|
Download a PICC information sheet here. A Peripherally Inserted Central Catheter (PICC) is a vascular access device inserted into a large vein in your upper arm and threaded to the superior vena cava, a large vessel above your heart. The PICC may remain insitu for weeks to months to years depending on the treatment and medications required. Use examples include:
Lab work can also be obtained from the line. The end of a PICC is always covered with a cap. When not in regular use, the line will be flushed weekly and a new cap applied. Once treatment is complete a PICC is easily removed by a certified nurse. |